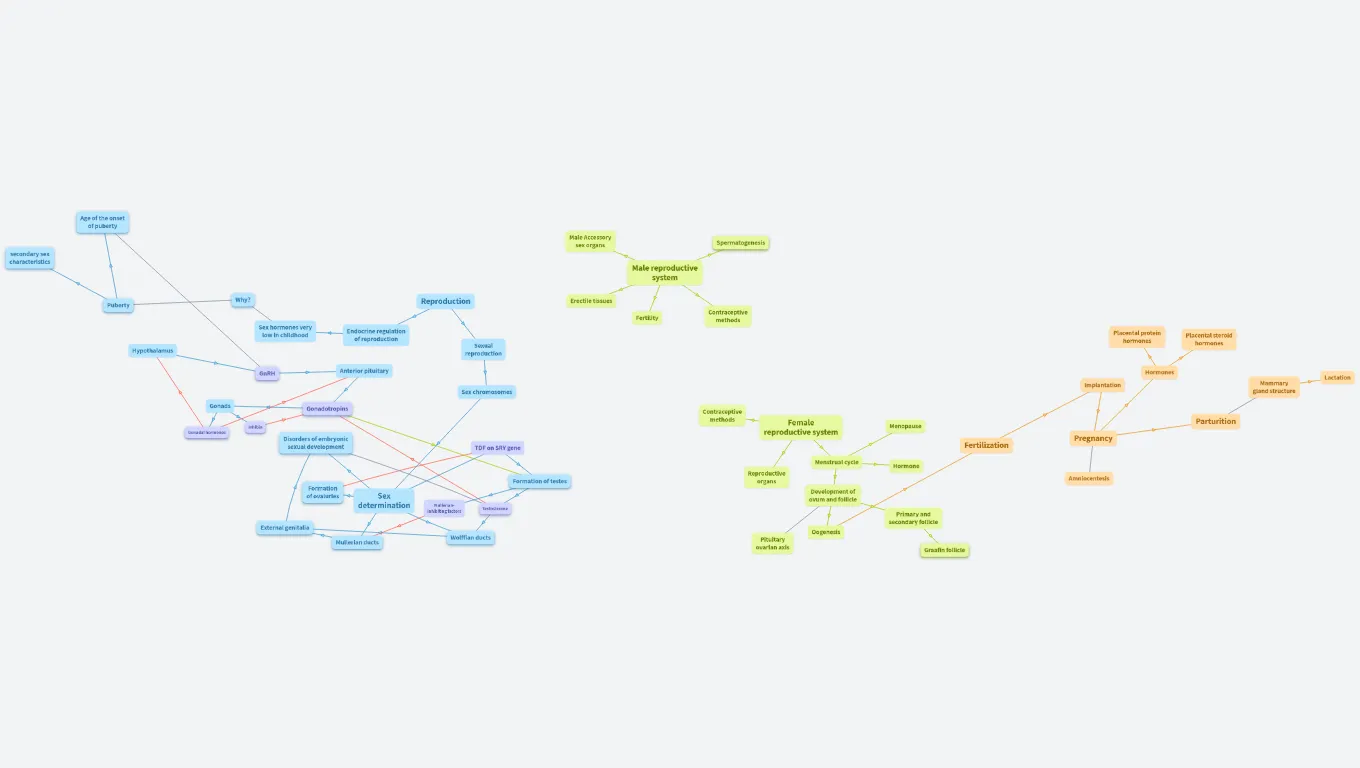
Reproduction
Created by Li Monnie
Age of the onset of puberty
Depends on the activity levels and body fat
- More activity→ inhibit GnRH secretion
- Leptin (protein) secreted by fat cells is required for puberty
secondary sex characteristics
Influence by
testestrone or estradiol-17β secretion
a. In girls: growth spurt, breast development,
menarche (first menstrual flow)
b. In boys: later growth spurt; body, muscle, penis,
and testis growth
c. In both sexes: body hair is stimulated by
androgens from adrenal gland at puberty
Male Accessory sex organs
Spermatogenesis
Spermatogenesis: Process of production or development of spermatozoa (stage 3→4)
Spermatogonia(2n)→ Spermatocytes(2n)/(1n)→ Spermatids(1n)→ Spermatozoa(1n)
Male reproductive system
Puberty
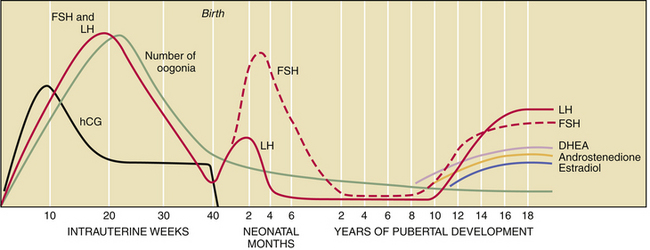
- FSH and LH secretion remains high for first 6 months, then decline until puberty
- Puberty begins with release of LH→ increase in (testestrone or estradiol-17β secretion)
→ Produce secondary sex characteristics
Why?
To have correct timing for puberty and secondary sexual characteristics development
Reproduction
Erectile tissues
Sex hormones very low in childhood
Fertility
Contraceptive methods
Hypothalamus
Endocrine regulation of reproduction
Sexual reproduction
Placental protein hormones
Placental steroid hormones
GnRH
- regulate FSH and LH
- pulsatory
Anterior pituitary
Hormones
Sex chromosomes
Implantation
Mammary gland structure
Lactation
Gonads
Gonadotropins
Hormones such as FSH and LH in both female and male, for:
- Stimulation of spermatogenesis or oogenesis
Stimulation of gonadal hormone secretion
Maintenance of the structures of the gonads
Testosterone: negative feedback on FSH and LH
Esteradiol: inhibit LH
Gonadal hormones
Male: testosterone
Female: estrogen, progestrone
Inhibin
- Secreted by Sertoli cells in testes
- Secreted by granulosa cells of ovarian follicles
- Specifically inhibits release of FSH (no effect
on LH)
Contraceptive methods
Disorders of embryonic sexual development
- Hermaphroditism: an ovary on one side and a testes on the other side; or have fused ovotestes.
Question: What determine a genetically male/female?
Ans: It involved complex factors such as DNA, internal gonads, external genitalia, etc, not only influenced by hormones.
- Pseudohermaphroditism: accessory structures are not complete or are inapropreiate for the genetic sex.
- Female Pseudohermaphroditism: congenital adrenal hyperplasia; exessive production of adrenal androgens (male sex hormone).
- Male Pseudohermaphroditism: due to malfunctionally testosterone receptors.
- Female external gentalia form, but internal mullerian ducts are degenerated
- Wollfian ducts also not stimulated
- Inability to produce emzyme 5⍺-reductace, which required for musclinization of external genetalia
Female reproductive system
Menopause
Pregnancy
Parturition
TDF on SRY gene
Menstrual cycle
Fertilization
Formation of testes
Seminiferous tubules form after production of TDF:
- Germinal cells: Spermatogonia
- Supporting cells: Sertoli cells
- make androgen-binding protein→ concentrate testosterone lv.
- Testosterone-producing: Leydig cells
Reproductive organs
Hormone
Formation of ovaluries
Without TDF, gonads of XX embryos develops into ovaries
Sex determination
Mullerian-inhibiting factors
Testosterone
Testosterone from Leydig cells stimulate the developement of wolffian ducts.
LH triggers secretion of testosterone
It contributes to muasculination, converted to DHT in brain cells by 5⍺-reductace or to estradiol by aromatase.
Question: Why testosterone need to be converted into DHT?
Ans: It has higher affinity for androgen receptors
- help develop and maintain of male secondary sexual characteristics
- differentiation of male external genitalia during fetal development
Development of ovum and follicle
Amniocentesis
External genitalia
They are identical for boy and girl in the first 6 months.
Primary and secondary follicle
Mullerian ducts
Becomes female tracts
Wolffian ducts
Become male tracts
Pituitary ovarian axis
Oogenesis
Graafin follicle
Mature follicle